[Article updated on 19/09/2023]
Diabetes, the scourge of modern times, is pushing us more and more to be concerned about our diet.
According to the WHO, this pandemic affects 3.3 million French people and 425 million people worldwide.
During my consultations, it is common to meet patients who have recently been diagnosed with diabetes. They are often surprised and do not know how to deal with this pathology.
It is undeniable that rapid dietary treatment is essential when diabetes is discovered.
What is diabetes ?
Diabetes is characterized by a chronic hyperglycemia, in other words a level of glucose (blood sugar) that is too high in the blood. Glucose is a simple sugar found naturally in food.
This hyperglycemia results from a disorder in the assimilation, use and storage of sugars provided by food.
What happens physiologically after a meal?
When we eat, one of the first steps of digestion allows carbohydrates to be transformed into glucose. Thus, the glucose formed leads to an increase in blood sugar levels. (= hyperglycemia phenomenon)
The pancreas then detects the increase in blood sugar. It goes, through certain cells called “ beta cells », secrete insulin.
The role of insulin is to bring glucose into the cells of the body, notably the muscles, adipose tissues and the liver where it will be transformed and stored.
Insulin is a hormone responsible in particular for regulating blood sugar levels. It is secreted continuously by beta cells located in islets of Langherans located in the pancreas. Depending on needs and the foods consumed, the body adapts its quantity of secretion.
This stage of insulin secretion allows a reduction in the quantity of glucose in the blood and therefore regulation of blood sugar levels.
In contrast to insulin, we find glucagon. Glucagon is a hormone also secreted by the pancreas. Its role, for its part, is to increase blood sugar levels. It will use the glycogen (glycogen is the result of the transformation of glucose by insulin) present in the liver to release it in the form of glucose into the blood. Its function is therefore opposite to that of insulin. Glucagon is particularly requested during exercise or intense fatigue.
On the pathological side
Unfortunately, it happens that in certain cases, insulin secretion is no longer adapted to needs (decreased or even non-existent).
This inadequate insulin response then prevents glucose from entering the cells. Glucose is forced to remain in excess in the blood, leading to chronic hyperglycemia or in other words, diabetes.
Some diabetes is preceded by an intermediate stage called “prediabetes”. During this phase, blood sugar levels are higher than normal but not high enough to establish a diagnosis of proven diabetes. Very often this stage precedes the imminent onset of type 2 diabetes, dietary management is therefore essential.
What are the different types of diabetes?
- Type 1 diabetes formerly called “insulin-dependent diabetes” is in the majority of cases discovered during childhood or adolescence. It represents 10% of diabetics.
T1D is an autoimmune disease. Indeed, we observe a destruction of the Langherans islands and therefore of the Beta cells by the organism itself. This results in an inability for the body to secrete the necessary amounts of insulin.
The symptoms of type 1 diabetes are specific; In particular, we observe intense thirst, abundant and frequent urine, as well as weight loss.
The only treatment is taking insulin (by injection or with an insulin pump).
- Type 2 diabetes is the most common form (around 90%). Unlike type 1 diabetes, type 2 most often appears after the age of 40.
T2DM is confirmed after three stages:
- Too frequent a state of hyperglycemia causes a significant and regular insulin response. As a result, tissues develop resistance to insulin, we then speak ofinsulin resistance.
Aging is a factor conducive to this insulin resistance ; however, this resistance is aggravated by a state of obesity/overweight. - The second stage is characterized by hyperinsulinism. The body attempts to overcome this resistance by increasing its secretion of insulin.
- After many years of chronic hyperglycemia, the pancreas will become exhausted and will no longer be able to secrete the necessary insulin in sufficient quantity. The quantity of insulin is deficient. We are talking of insulin deficiency.
The genetic causes of the appearance of T2DM are in the minority. Being overweight, an unbalanced diet and a lack of physical activity are factors favoring T2DM.
Dietary support is then essential. Treatment with oral or injectable antidiabetics can be implemented. Insulin injections are used as a last resort, if the disease is too advanced.
- Gestational diabetes is discovered during pregnancy.
This type of diabetes can, however, exist well before pregnancy and reveal itself during blood tests.
In most cases, dietary measures are sufficient. If blood sugar levels are unstable and become dangerous for the pregnant woman, then insulin may be necessary. This type of diabetes normally disappears after childbirth if dietary monitoring is ensured.
The consequences for the baby and for the pregnant woman can be multiple: Pregnancy-related hypertension, pre-eclampsia, premature delivery, renal failure, fetal macrosomia, etc.
- Diabetes Mody (Maturity Onset Diabetes of the Young) constitutes one of the rarest forms of diabetes (2%).
There are six different forms depending on the mutation of the gene concerned.
Its origin is therefore genetic and mainly concerns young, non-obese subjects.
The therapy is more similar to T2D, initially with nutritional support and, depending on the progress of the disease, taking antidiabetics or even insulin.
- Type 3 diabetes “diabetes of the brain”
Recent studies show a link between diabetes and Alzheimer’s disease.
Insulin receptors are present in the brain; thus in case of diabetes; these cells cannot be nourished by glucose. This phenomenon contributes to the degeneration of certain neurons, particularly in the context of Alzheimer’s disease.
People with T2D have a 50% increased risk of developing Alzheimer’s.
In addition, patients with Alzheimer’s disease may have a loss of insulin sensitivity. It is therefore an old circle between these two pathologies.
Surveillance for these two diseases must be very high.
The consequences of all these types of diabetes are multiple and can be extremely serious: Cardiovascular diseases, eye disorders, neuropathies, susceptibility to infections, etc.
Hygiene and dietetic measures
Physical activity is a factor that should not be neglected when managing diabetes. It contributes on various points:
- Reduction in fat mass
- Increased body sensitivity to insulin (GLUT4)
- Reduction in cardiovascular risks
- Weight control
- Reduced cholesterol and triglycerides
- Decrease in glycated hemoglobin
- Stress reduction
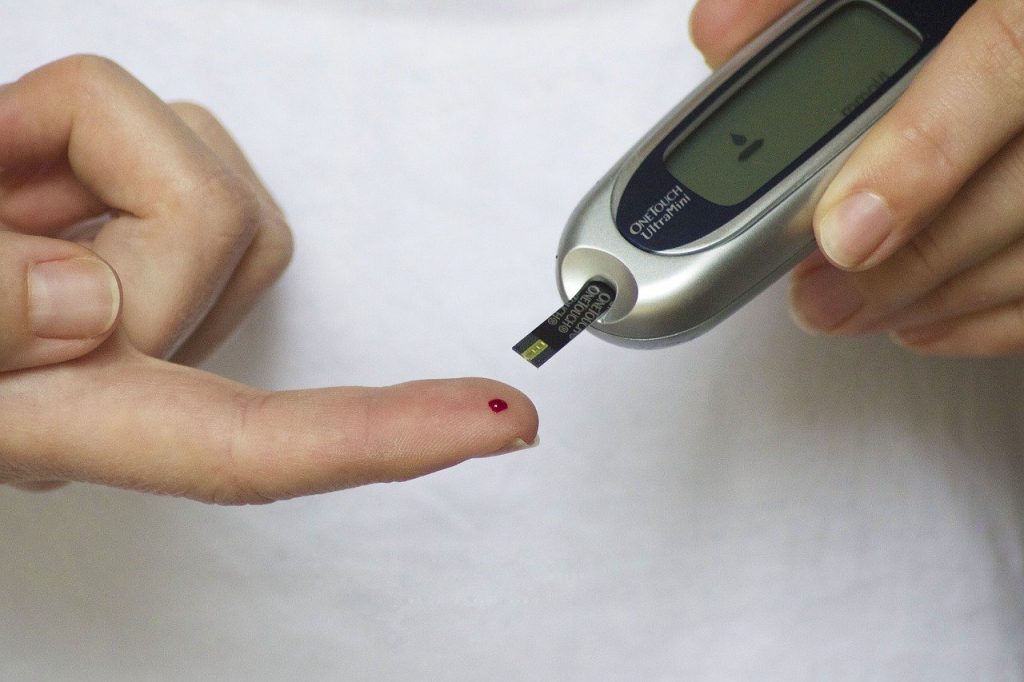
Physical activity must, of course, be adapted according to the patient’s pathology. Learning to control your blood sugar is essential when exercising in order to avoid the risk of hypoglycemia which can be fatal.

From a nutritional point of view
The diet of a diabetic must be fundamental to his therapy.
So, the ideal is to always start your meal with a raw vegetable. In fact, the fibers contained in raw vegetables limit a rise in blood sugar levels. In addition, the high content of vitamins and minerals is interesting to compensate for the risks of deficiencies.
The structure of the dish must, for its part, be divided into three parts:
- A portion of animal proteins (meat/fish/egg) representing approximately 1/3 of the plate. Proteins, in addition to their satiating effect, have a fundamental role for the body, particularly for the maintenance of muscle tissues.
- A portion of starchy foods. Ideally 1/3 of the plate. Whole starchy foods should be favored, particularly due to their high fiber content. The quantities of starchy foods consumed at each meal should be as equal as possible in order to stabilize blood sugar levels.
- A portion of vegetables representing ½ of the plate. A meal rich in vegetables delays the absorption of carbohydrates and contributes to the prevention of cardiovascular diseases.
As for dessert, the ideal is to combine a dairy product with a “raw” fruit.
In order to limit variations in blood sugar, foods with a low glycemic index should be favored.
The glycemic index is the ability of a food to increase blood sugar levels after absorption.
| Low GI foods | High GI foods |
| – Agave syrup – Raw fruits (apples, oranges, pears, bananas) – Green vegetables – Dried vegetables and legumes (red beans, white beans, lentils, chickpeas, split peas, etc.) – Quinoa, bulgur – Wholemeal pasta cooked “al dente” – Complete rice – Potato in cold salad – Sourdough wholemeal bread | Sugar and sweet products (pastries, pastries, etc.) Compote (cooking + grinding) Dried fruits (to combine with oilseeds) Pressed fruits Ordinary pasta -> pasta gratins White rice, quick cooking rice Steamed potato, fries White bread, sandwich bread, rusks |
Advice
- Most often consume “raw” (whole) foods: avoid overcooking them, mixing them, pressing them
- Always mix starchy foods with double the quantity of vegetables to reduce the glycemic index of the meal.
It is important to never consume sugary products in isolation to avoid hyperglycemia. You must systematically combine a sweet product with a dairy product or a complete starch.
Regarding drinks, water is of course the drink of choice. Alcohol, sodas or other sugary drinks have a significant impact on raising blood sugar levels. Therefore, it will be better to consume them during a meal.
“It’s not sugar that causes diabetes. The diabetic diet is a normocaloric and balanced diet. This means that the diabetic must eat as we all should, and if the diabetic has a particular diet, it is because the rest of the population eats too poorly” Dr Michel Cavey – diet of the elderly-famidac-March 2008.
